The Lure of Best Practice – The Next Shining Object Challenge
Feb 18, 2026
Healthcare organizations love best practices. They attend conferences, compare dashboards, and borrow workflows that worked somewhere else. On paper, it makes sense. If it worked there, it should work here.
Afterall who doesn’t want to do things “the best, most efficient way”. But this is actually like saying one diet plan fits everyone trying to get healthy. It just doesn’t work that easily.
I’ve sat in countless leadership meetings that all start the same way. Finance is focused on accounts receivable and cash flow. Clinical leaders are frustrated by disrupted schedules and the loss of momentum that comes with constant workflow changes. Compliance is tracking documentation gaps that feel invisible until they suddenly matter.
Same organization. Three very different realities.
No one is wrong.
They just aren’t aligned.
This is where improvement efforts quietly stall. The best advice still applies. Do not make the mistake of trying to put a square peg in a round hole.
When organizations reach for “best practices” too early, they skip the most important step: understanding how their own systems actually work together now. Without that clarity, even strong solutions feel disruptive. Teams push back. Metrics don’t move. Leadership wonders why change never seems to stick.
What I’ve seen work looks much less flashy. Its actually hard work and people have to be willing to be vulnerable to open discussion exposing problems at the root.
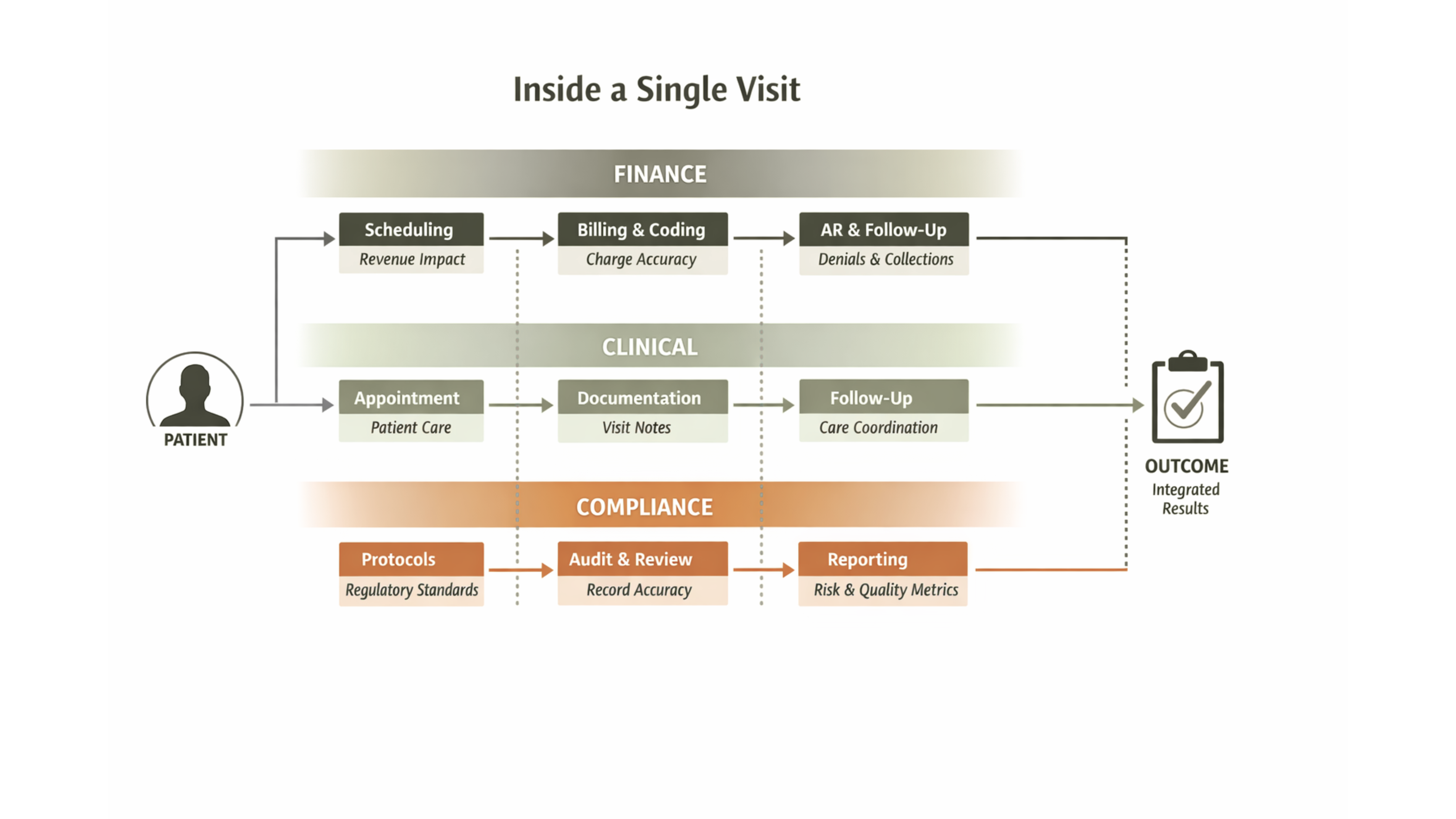
Instead of starting with benchmarking, the organizations that make real progress start by bringing finance, clinical, billing and compliance leaders into the same conversation. Not to defend their departments. Not to assign blame. But to walk through how a single visit moves through the organization from scheduling to documentation to billing.
That exercise is where the real issues surface.
Schedules don’t just break down because of no-shows. They break down when workflows are rigid, expectations are unclear, and work continues even when the visit doesn’t. Clinicians don’t just lose visits they lose rhythm. Documentation doesn’t disappear. Administrative tasks still need to be completed. Frustration builds quietly, often long before anyone calls it burnout.
When leadership sees this together, something shifts.
The conversation moves away from “your problem” and toward “our process.” Teams start to see how financial pressure, clinical reality, and compliance expectations intertwine in ways that no single department can fix alone. Solutions emerge organically not because someone imposed them, but because everyone finally sees the same picture.
This is also where no-shows stop being just a metric. They become a signal. A signal that something in the system isn’t working as smoothly as it should for patients and for staff.
Only after that internal alignment does it make sense to look outward.
Best practices are powerful when applied at the right time. But when organizations borrow solutions before understanding their own friction points, they end up layering complexity on top of confusion.
Best practice doesn’t fail because it’s wrong.
It fails because it’s applied too early.
Internal alignment is the real starting line. I encourage organizations to do the hard work first then bring in the next shiny best practice plan. You have to understand the root of your problem but you don’t have to reinvent the solution.